Key Takeaways
- BIPOC communities face significant barriers to mental health care, with only 25-33% receiving treatment compared to 50% of white adults
- Cultural competence in therapy requires understanding historical trauma, code-switching, and systemic inequalities
- Finding a culturally competent therapist involves looking for specific training, cultural humility, and representation
- Mental health stigma in BIPOC communities often stems from historical mistreatment and protection instincts
- Effective therapy for BIPOC must honor both cultural traditions and individual healing needs
Mental health matters to everyone, but not everyone gets the same care. In the United States, people of color often face more barriers to getting help, more stigma when they try, and more pain that goes untreated.
Ready to Find Culturally Competent Care?
To understand why, we have to look at where therapy came from, and who it left out.
Therapy's Complicated Past
Modern talk therapy began in Europe with ideas from white male thinkers like Freud and Jung. Early mental health institutions were not made for healing, they were made to control and isolate people. For example:
- Women who acted “too emotional” were often labeled with “female hysteria.”
- Homosexuality was once called a mental disorder. (APA, 2013)

These histories matter because they show us the roots of how therapy was shaped, and who was seen as needing “fixing.”
Medical textbooks from the past also made racist claims. They said Black people had higher pain tolerance or smaller skulls, ideas we now know are false and harmful (Hoffman et al., 2016). These lies created deep mistrust. That mistrust still shows up today in many BIPOC communities.
When we say mental health care should be fair, we’re not just asking for more therapists, we’re asking for a new kind of care. One that sees history. One that hears people. One that heals without judgment.
Living Two Lives: Cultural Identity and Code-Switching
If you’re a person of color, you might already know what it means to live two lives. One at home, shaped by family and culture. One in public, shaped by pressure to fit in.
This balancing act is called code-switching. It can be exhausting. A client might speak freely in their mother tongue at home but feel nervous to speak at work. Or someone might laugh off racy jokes just to “keep the peace,” even though it hurts.
Therapy must understand that this “double life” can be exhausting and in some cases debilitating. And if therapists don’t see that, clients may feel invisible or misunderstood.
Why BIPOC Don't Trust Therapy
Many BIPOC families carry stories of mistreatment by medical systems. One of the most infamous examples is the Tuskegee Syphilis Study (Centers for Disease Control and Prevention [CDC], 2022), where Black men were told they were receiving free treatment but were actually being used for medical experiments without their knowledge.
These histories don’t just disappear. They live on in cultural memory. When someone from an older generation warns, “Don’t trust doctors,” that fear didn’t come from nowhere.

This is why mental health stigma can be stronger in these communities. It’s not just about shame. It’s about protection.
A Real-Life Example: Who Gets Diagnosed?
Black boys are more likely to be labeled with Oppositional Defiant Disorder (ODD) (Gibbs et al., 2013). But what if those behaviors, like not trusting teachers or acting out, come from trauma or feeling unsafe?
When kids push back against systems that don’t treat them fairly, they’re often punished instead of understood.
That’s why culturally competent therapy matters. Because diagnosis without context isn’t care, it’s harm, causing a potential cascade of labeling and feeding into the cycle of mistreatment. Children live to the expectations we put for them, given the expectation of ODD will lead to over analysis ever act as one from the frame of defiance rather than a child practicing autonomy.
Systemic Inequality Isn't Just Background Noise
Therapy often focuses on helping the individual. But what about the world around them?
A therapist can’t ignore poverty, racism, or unsafe schools. Telling someone to “just set boundaries” may not work when their whole family shares one apartment. Saying “cut off toxic family” may not help in cultures where family is survival.
In many BIPOC families, pain is passed down. So is strength. Therapy should honor both.
When Peace Feels Dangerous
In some communities, survival has meant being tough. Vulnerability can feel unsafe. Some youth fear that if they stop pushing so hard, they’ll fall apart. They say, “If I rest, I’ll break.”
One client once said, “Peace will kill me.” That sentence holds more truth than any diagnosis ever could.
This isn’t just about individual choice—it’s about what happens when generation after generation has been forced to focus on survival. When your grandmother had to fight for basic safety, when your father learned that vulnerability meant danger, when your community has been told that rest is a luxury they can’t afford.
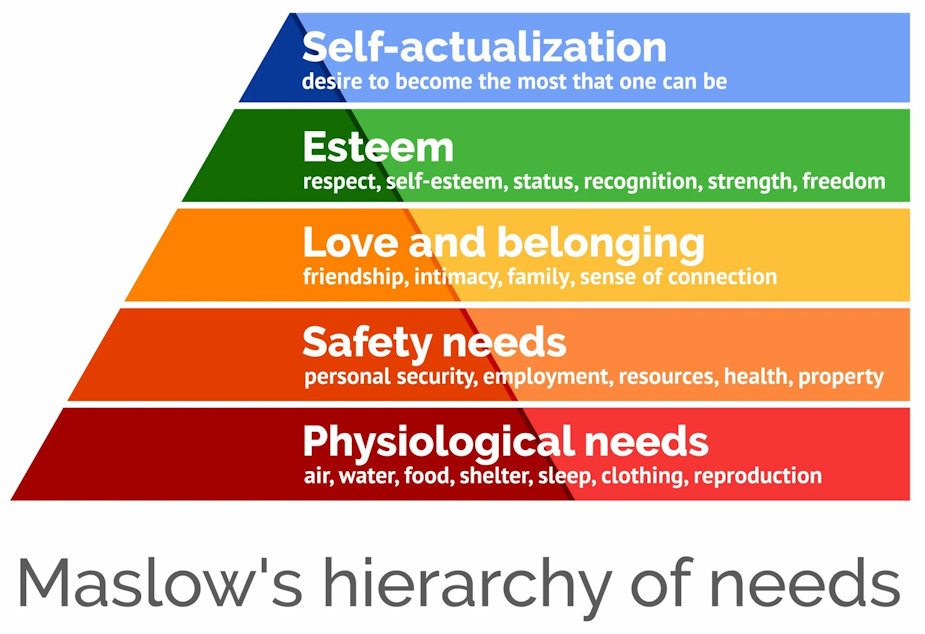
Think about Maslow’s hierarchy of needs. When families spend decades stuck at the bottom fighting for physiological needs and safety, it becomes almost impossible to climb toward love, esteem, and self-actualization. How do you work on self-esteem when you’re still worried about where your next meal is coming from? How do you focus on personal growth when your nervous system is still wired for survival?
Research shows that trauma doesn’t stop with those who suffered it directly. Your stress tolerance, your relationship with vulnerability, even your ability to trust peace—these can all be shaped by experiences you never lived through. Mark Wolynn’s work in “It Didn’t Start With You” explores this phenomenon of intergenerational trauma, showing how the wounds of previous generations can live on in our nervous systems and behaviors.
So when someone says “peace will kill me,” they’re not being dramatic. They’re speaking from a place where peace has historically meant letting your guard down—and letting your guard down has meant getting hurt. Their nervous system has learned that constant vigilance is the price of survival.
This is why culturally competent therapy matters so much. A therapist who doesn’t understand this history might see someone’s resistance to relaxation as a problem to fix. But a culturally competent therapist understands that this resistance is often wisdom—hard-won wisdom passed down through generations who learned that vulnerability was dangerous.
The work isn’t about forcing someone to trust peace. It’s about creating enough safety that peace can become an option. It’s about honoring the survival strategies that kept families alive while gently opening space for something different.
Mental Health Gaps in Numbers
Treatment Rates by Race/Ethnicity?
- Almost 50% of white adults with mental illness receive treatment
- Only 33% of Latinx adults do
- Only 31% of Black adults do
- Only 25% of Asian Americans and Pacific Islanders do
(National Alliance on Mental Illness [NAMI], 2023)
Among youth:
- 76% of Black children with mental health needs receive no professional help (Mental Health America, 2023)
- In some cities, that number is even higher
Suicide rates are rising in Black teens, but many still don’t get therapy. Why? Stigma. Mistrust. Cost. Lack of providers who look like them or understand their stories.
Among youth:
- 76% of Black children with mental health needs receive no professional help (Mental Health America, 2023)
- In some cities, that number is even higher
Suicide rates are rising in Black teens, but many still don’t get therapy. Why? Stigma. Mistrust. Cost. Lack of providers who look like them or understand their stories.
It's Not Just a Lack of Access, It's a Lack of Safety
Even when care is available, it often isn’t culturally safe. Therapists may misunderstand the role of religion, ignore racism, or assume every family values independence over community (Sue et al., 2009).
That’s why therapy must be culturally competent. And that’s why representation matters.
Currently:
- Only 2% of psychiatrists and 4% of psychologists in the U.S. are Black (American Psychiatric Association, 2022)
- Many BIPOC clients say they’ve had to teach their therapist about their culture. That’s exhausting. And unfair.
What Helps? Finding a Culturally Competent Therapist
Not every therapist will be the right match—and that’s okay. What matters is finding someone who respects your story, your culture, and your truth. Use the checklist below to help you find a therapist who’s culturally competent, safe, and ready to support you.
Everyone worries sometimes; that’s just being human. But how can you tell when your anxieties have crossed over from everyday worry into something debilitating? To help, I want you to explore with yourself; What Could Happen vs What Will Happen 
Download Your Therapist Checklist
Therapy for Black Girls
Latinx Therapy
Asian Mental Health Collective
Indigenous Circle of Wellness
National Queer and Trans Therapists of Color Network
The Steve Fund
Final Thoughts: Culture is Not the Problem, It's Part of the Solution
Therapy doesn’t work when people feel unseen. BIPOC clients don’t need saviors—they need allies. They need therapists who will listen without judgment, understand their cultural context, and help them carry what’s too heavy to hold alone.
We’re not just individuals. We’re families. We’re communities. And our mental health is shaped by all of it.
Healing can look different. It can happen in a circle. It can happen in a song. It can happen in a story told by a grandmother. It can happen in therapy—when therapy is done right.
Culturally competent care isn’t “extra.” It’s essential.
Ready to Find Culturally Competent Therapist?
FAQs About Culturally Competent Therapy
Culturally competent therapy is mental health care that understands and respects a person's cultural background, experiences, and identity. For BIPOC communities, this matters because:
- Historical mistrust: Many BIPOC families carry stories of medical mistreatment, like the Tuskegee Syphilis Study, creating lasting barriers to seeking help
- Cultural context: Therapy must understand code-switching, family dynamics, and systemic inequalities that shape mental health
- Representation gaps: Only 2% of psychiatrists and 4% of psychologists in the U.S. are Black, making it harder to find providers who understand your experiences
- Treatment disparities: While 50% of white adults with mental illness receive treatment, only 25-33% of BIPOC adults do
Effective culturally competent therapy honors both cultural traditions and individual healing needs, recognizing that culture is not the problem—it's part
Finding the right culturally competent therapist involves research and asking the right questions:
- Look for specific training: Check if they mention "cultural humility," "anti-racism," or "trauma-informed care" in their credentials
- Research their background: Do they mention working with BIPOC clients in their bio? Are they part of diversity-focused networks?
- Ask about cultural understanding: During initial conversations, see if they ask about your cultural background and are open to discussing experiences with racism, faith, or family roles
- Watch for red flags: Avoid therapists who ignore race/culture completely, say "I don't see color," or seem uncomfortable discussing identity issues
Use the interactive checklist in this article to evaluate potential therapists and ensure they're truly culturally competent.
BIPOC communities face multiple barriers to mental health care:
- Historical trauma and mistrust: Centuries of medical experimentation and mistreatment have created deep-seated distrust in healthcare systems
- Cultural stigma: Mental health stigma in BIPOC communities often stems from protection instincts and historical mistreatment
- Systemic inequalities: Poverty, racism, and unsafe environments create barriers that go beyond individual therapy needs
- Lack of representation: With only 2-4% of mental health professionals being Black, many BIPOC clients struggle to find providers who understand their experiences
- Economic barriers: Cost and lack of insurance coverage prevent many from accessing care
- Cultural misunderstandings: Traditional therapy approaches may not align with cultural values around family, community, and healing
Start small: turn off notifications, set time limits, and take breaks before bed. Try "tech-free zones" like no phones at the dinner table or in the bedroom. Use apps or timers to help stay on track.
- Misdiagnosis patterns: Black boys are more likely to be labeled with Oppositional Defiant Disorder (ODD), but these behaviors often stem from trauma or feeling unsafe rather than defiance
- Cultural bias in assessment: Standard mental health assessments were developed primarily for white populations and may not account for cultural differences in expression and coping
- Provider bias: Unconscious bias can lead to different treatment recommendations or assumptions about BIPOC clients' needs
- Context blindness: Therapists may focus on individual symptoms while ignoring systemic factors like racism, poverty, or unsafe environments that contribute to mental health challenges
- Treatment approach mismatch: Western individualistic therapy models may conflict with collectivist cultural values common in many BIPOC communities
Works Cited
- National Alliance on Mental Illness. (2023). Mental health facts in diverse populations.
- Pinedo, M., et al. (2021). Immigration enforcement and mental health. American Journal of Community Psychology.
- Manalo-Pedro, E., et al. (2024). Anxious Activists? Immigration policy threat and mental health. Social Science & Medicine.
- U.S. Department of Health and Human Services. (2022). Mental health disparities: African American populations.
- Mental Health America. (2023). Access to care data.
- APA. (2020). Understanding race and privilege.